Why Diabetic Patients Should Avoid Thin-Sole Slippers | Diabetic Foot Care
People living with diabetes often focus on sugar control, diet, and medication, but foot care is just as important. One small mistake—like wearing thin-sole slippers daily—can lead to serious foot problems. Many diabetic patients prefer thin slippers because they feel light and comfortable, but in reality, they can silently damage your feet over time.
This blog explains why diabetic patients should avoid thin-sole slippers and how choosing the right diabetic footwear can protect your feet and overall mobility.
How Diabetes Affects Your Feet
Diabetes can cause two major foot-related problems:
1. Diabetic Neuropathy (Nerve Damage)
Reduced sensation in the feet makes it difficult to feel pain, heat, cuts, or pressure. Small injuries often go unnoticed and worsen over time.
2. Poor Blood Circulation
Diabetes slows down healing. Even minor wounds can turn into serious infections or ulcers.
Because of these risks, footwear plays a critical role in preventing complications.
What Are Thin-Sole Slippers?
Thin-sole slippers usually have:
-
Very little cushioning
-
No shock absorption
-
Flat, flexible soles
-
Minimal foot support
They are commonly used at home and outdoors because they are easy to wear—but they are unsafe for diabetic feet.
Why Thin-Sole Slippers Are Dangerous for Diabetic Patients
1. No Protection From Pressure Points
Thin soles do not distribute body weight evenly. Continuous pressure on one area can lead to calluses, corns, and foot ulcers—especially dangerous for diabetic patients.
2. Higher Risk of Foot Injuries
Sharp objects, stones, uneven surfaces, or hot floors can easily injure the foot. Due to reduced sensation, these injuries may go unnoticed until infection develops.
3. Poor Shock Absorption
Every step creates an impact on your heels and forefoot. Thin soles fail to absorb shock, increasing stress on joints, nerves, and soft tissues.
4. Increased Risk of Cracks and Ulcers
Hard floors and lack of cushioning cause excessive dryness and heel cracks. Cracked skin can allow bacteria to enter, leading to infections.
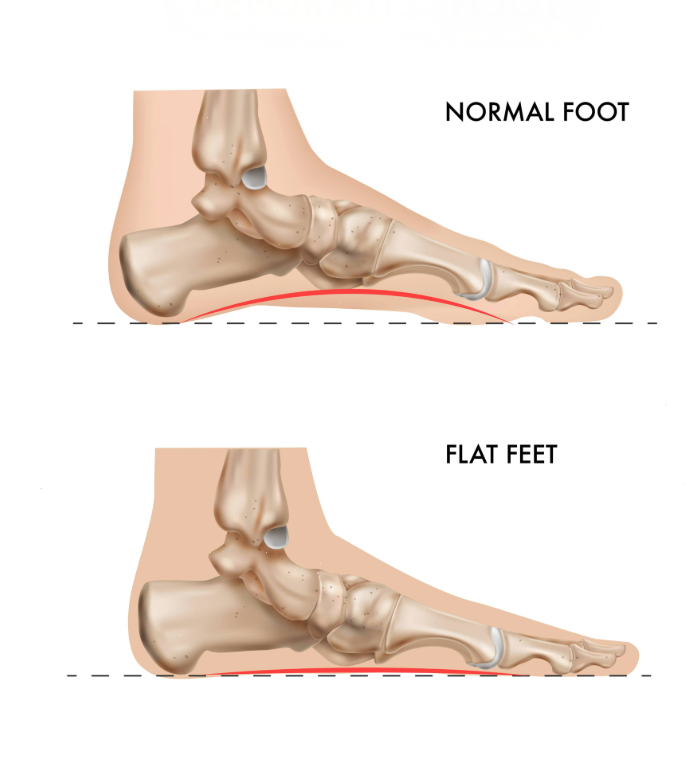
5. No Arch or Heel Support
Thin slippers provide no structural support, increasing foot fatigue, imbalance, and the risk of deformities like plantar fasciitis or collapsed arches.
Common Foot Problems Caused by Thin-Sole Slippers
-
Diabetic foot ulcers
-
Heel cracks and fissures
-
Corns and calluses
-
Foot infections
-
Increased risk of amputation in severe cases
These problems often start small but can become life-threatening if ignored.
What Kind of Footwear Should Diabetic Patients Choose?
Instead of thin-sole slippers, diabetic patients should use orthopedic or diabetic footwear with the following features:
Cushioned, Thick Sole
Absorbs shock and protects feet from hard surfaces.
Pressure-Relieving Insole
Distributes body weight evenly to avoid pressure points.
Anti-Slip Outsole
Prevents falls and injuries.
Soft, Seam-Free Inner Lining
Reduces friction and prevents skin damage.
Proper Arch and Heel Support
Maintains correct foot alignment and reduces strain.
Breathable Materials
Keeps feet dry and reduces the risk of fungal infections.
Can Diabetic Patients Wear Slippers at Home?
Yes—but only diabetic-friendly slippers designed with orthopedic support. Even at home, barefoot walking or thin slippers should be avoided, as most foot injuries happen indoors.
Frequently Asked Questions (FAQs)
Q1. Are thin slippers safe for short indoor use?
No. Even short-term use can cause injuries that diabetic patients may not feel immediately.
Q2. What is the best footwear for diabetic patients at home?
Diabetic slippers with cushioned soles, arch support, and soft inner lining are ideal.
Q3. Can thin soles cause diabetic foot ulcers?
Yes. Continuous pressure and unnoticed injuries from thin soles can lead to ulcers.